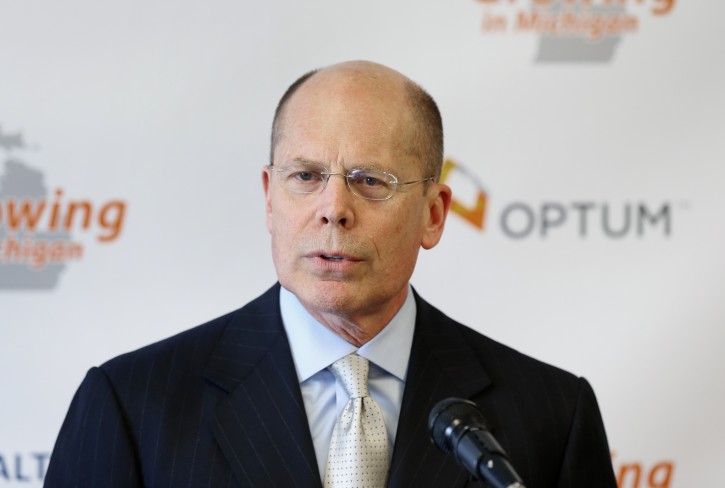
New York – UnitedHealth CEO Stephen Hemsley offered a mea culpa Tuesday for his company’s decision to dive deeper into the Affordable Care Act’s public insurance exchanges, a move that ultimately forced the nation’s largest health insurer to cut its earnings forecast.
Hemsley told investors that the insurer should have learned more about the still-new business, and expanding before it did that was “for us, a bad decision.” UnitedHealth jumped into two dozen state-based exchanges for 2015 after selling coverage on just four in 2014.
“It will take more than a season or two for this market to develop,” Hemsley said during a webcast of the company’s annual meeting with investors in New York.
UnitedHealth lowered its 2015 outlook last month after detailing steep losses from the exchange business. The insurer also said its exchange business — a small slice of its overall portfolio — was weighing on its 2016 earnings forecast, and it would decide next year whether to even participate in the exchanges in 2017.
That announcement shook health insurance stocks and raised concern about the long-term viability of the state-based insurance exchanges, a key component of the overhaul’s push to expand coverage to millions of uninsured people. Several smaller, nonprofit insurance cooperatives also have said that they would stop selling coverage on the exchanges for 2016.
But UnitedHealth’s forecast revision last month also prompted several rivals to reaffirm their own outlooks and their loyalty to the exchanges.
Hemsley said Tuesday that “time will tell” whether the exchanges can eventually yield a viable business for UnitedHealth.
Insurers have struggled, in general, to attract and keep enough premium-paying healthy customers to their exchange coverage to balance those who use more health care.
Hemsley said UnitedHealth tried to grow conservatively, by selling coverage in markets where it already had a network of established service providers. But the exchange business has been hurt in particular by customers who signed up for coverage outside designated enrollment windows and then submitted a lot of medical claims.
Insurers also say they’ve been hurt to a lesser extent by customers who sign up for coverage and then stop paying their premiums.
“We did not believe it would form this slowly, be this porous or become this severe,” Hemsley said.
The CEO said his company will narrow decisions on whether to stay in the exchanges down to individual products and markets.
“We will not knowingly lose money on this product line in 2017,” he said.
He added that any decisions on the exchange business may not be permanent. Hemsley noted that the Minnetonka, Minnesota-based insurer pulled back from the market for Medicare-related coverage in 1999 but now has a large presence in that business.
Health insurance is UnitedHealth’s largest business by far, but the company also has been touting its growing Optum segment, which provides pharmacy benefits management and technology services and runs clinics and doctor’s offices
Overall, the insurer expects 2016 earnings of $7.10 to $7.30 per share on revenue ranging from $180 billion to $181 billion.
Analysts forecast, on average, earnings of $7.21 per share on $183 billion in revenue, according to FactSet.
Shares of UnitedHealth climbed almost 2 percent, or $2.11 to $114.82 in midday trading Tuesday, while broader indexes were up less than 1 percent.
As reported by Vos Iz Neias
