Within a decade, manufactured hearts could obviate the need for organ donations, but ethicists warn of pitfalls along the way
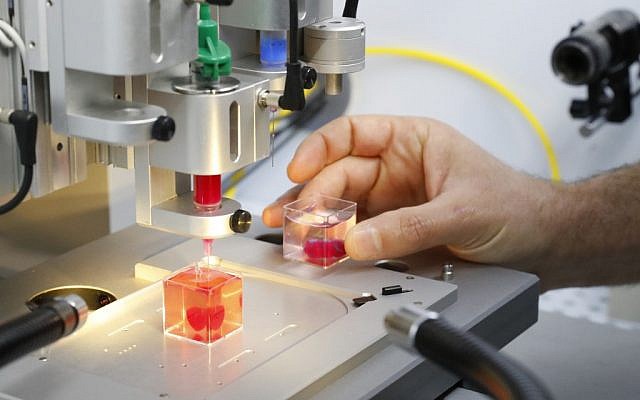
At a Tel Aviv fruit and vegetable store on Monday night, shoppers suddenly stopped what they were doing to stare at a television screen overhead. The television news anchor was announcing a medical breakthrough: a team of researchers from Tel Aviv University had 3D-printed a heart using a patient’s own cells and biological material.
“The future is here,” one shopper remarked to another.
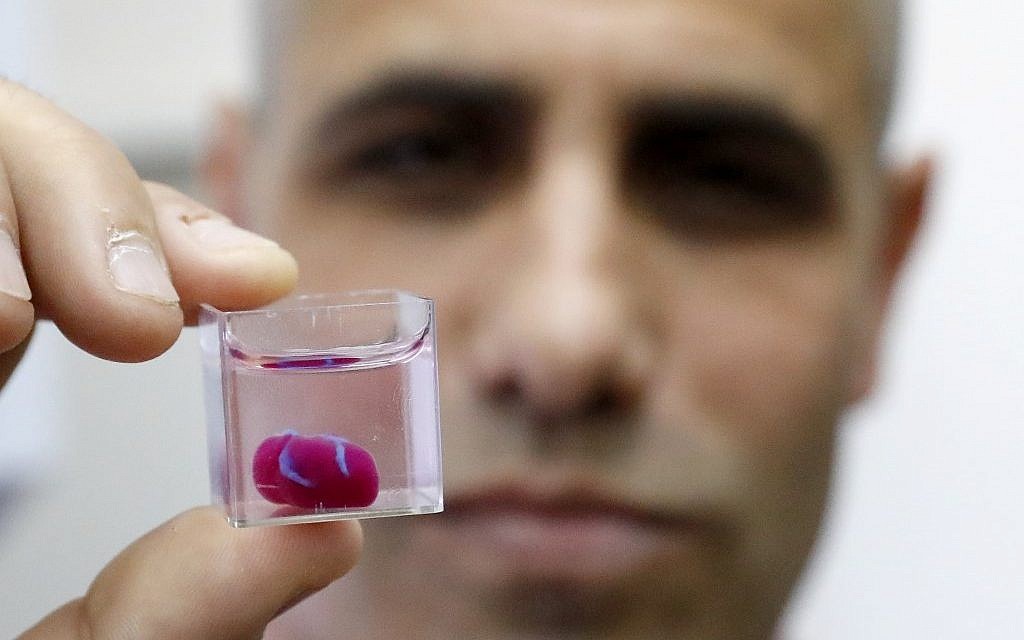
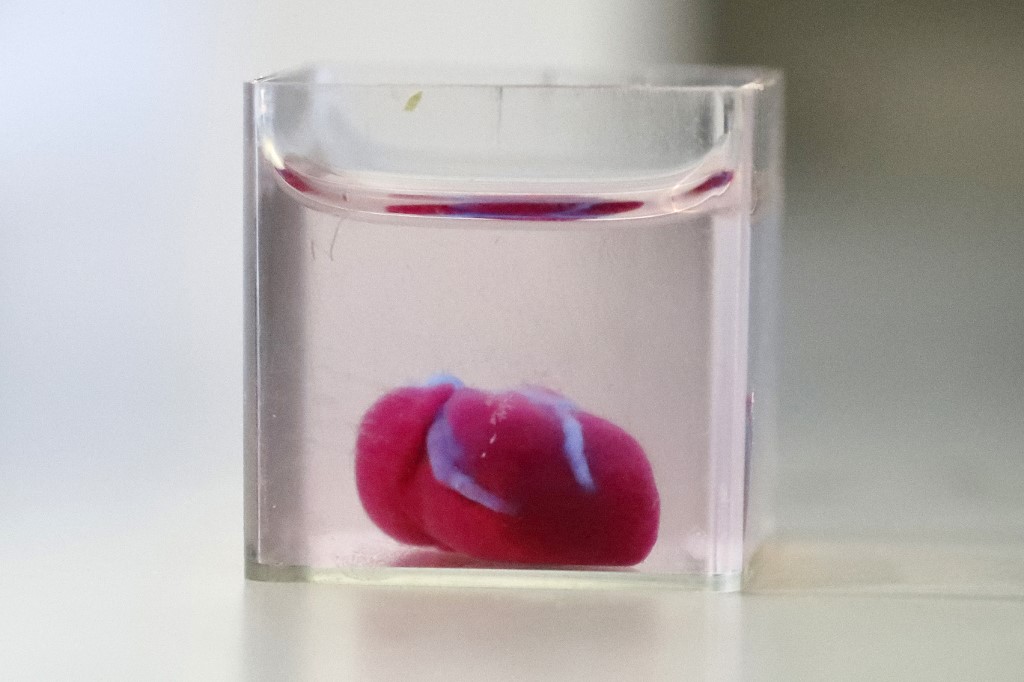
Israelis are swelling with pride at the scientific breakthrough revealed at a press conference on April 15 and in a paper in the peer-reviewed journal Advanced Science. Until now, scientists have been able to 3D print simple tissues without blood vessels, but the Israeli team, led by Prof. Tal Dvir of TAU’s School of Molecular Cell Biology and Biotechnology, has printed an entire heart including cells, blood vessels, ventricles and chambers.
The grape-size heart shown at Tel Aviv University does not work yet. It needs to be matured in a bioreactor, where electrical and mechanical signals will coax the cells into contracting synchronously, a process that will take about a month. Researchers also need to figure out how to generate more and bigger cells so that they eventually can 3D print a human-size heart, which contains billions of cells. They also have yet to transplant a heart into animals which will eventually be followed by clinical trials on humans.
This breakthrough, Dvir estimated, is likely to lead 3D-printed human hearts in hospitals within a decade.
But not everybody is gung-ho about the heart breakthrough, citing ethical implications, like whether it will widen the gap between rich and poor and whether superhuman hearts or other mutations can also be manufactured.

Robby Berman, director of the Halachic Organ Donor Society told The Times of Israel he had mixed feelings about the Tel Aviv University announcement, mostly because people might think they no longer need to donate organs.
“The artificial heart is good in that it shows we are progressing that one day we will be creating organs to save lives,” said Berman.
Berman pointed out that only 16 percent of Israelis have signed organ donor cards (compared to 50% in the United States) and that while the Tel Aviv University breakthrough may one day ameliorate Israel’s organ shortage, that day is a long way off.
“ I hope this doesn’t send the untrue message that we are just a few years away from artificial organs because we are not. People still need to have the conversation with their families and let everyone know — family and friends — that they want to be an organ donor.”
Dr. Rabbi Ira Bedzow, director of the Biomedical Ethics and Humanities Program at New York Medical College told The Times of Israel that whenever there is a new medical discovery, both those who view its potential as utopian and those who fear its unintended consequences are failing to grasp the complexity of the situation.
“My assumption is that if this works it is going to be life-saving,” Bedzow said. “What it’s going to end up doing is addressing the issue of organ shortages, and it’ll also be easier for the patients because the patients won’t have to worry about organ rejection, or Graft Versus Host disease, or taking immunosuppressants because the cells the organ is made of are going to be from their own body.”
However, Bedzow said there are potential pitfalls involved with categorizing the organs as body parts or medical devices. If they are organs, they can’t be bought and sold and no one owns them, according to the law in most countries. This would probably keep the cost of such organs low and prevent other abuses.
But if they are categorized as medical devices, they can be patented and the owner of the organs could conceivably charge a lot of money for his product, rendering it unaffordable to many unless covered by insurance.
Another related question is whether a patient will sell the rights to her genetic material to the company printing the heart. Would the company then be able to create more hearts using her cells or use her cells for other purposes? In the United States, for instance, a person’s genetic material is owned by them and a research or medical facility must get their consent if they want to use it in any way, he said.

Bedzow said the problem of organs being considered medical devices is doubly problematic because the medical devices industry itself has been an object of controversy.
A November 2018 series of exposes by the International Consortium for Investigative Journalists revealed how “health authorities across the globe have failed to protect millions of patients from poorly tested implants that can puncture organs, deliver errant shocks to the heart, rot bones and poison blood, spew overdoses of opioids and cause other needless harm.”
In March, the Department of Homeland Security warned that certain heart implants were hackable from a short distance.
“There is a rush to innovation that sometimes has had very bad consequences for patients,” said Bedzow. “It’s one of the problems that we have of looking at helping patients as a public good but then privatizing a lot of these markets where players seek financial gain.”
Bedzow said that people creating medical devices need to “recognize their mission as much as their margin” and that medicine should be a public good and not merely a good or service bought and sold in a market like potato chips and clothing.
Superhuman hearts
As for whether customizable 3D-printed organs could lead to a community of large-hearted superhumans, Bedzow said there was little reason to worry.
If a doctor put a “superheart” into someone’s body, it wouldn’t make a huge difference to their overall health and longevity because it has to work within the rest of the person’s cardiopulmonary systems. Even if a doctor were to hypothetically replace all of a person’s major organs with 3D-printed ones it might add another 20 years to their life, Bedzow said.
“I’d be more worried about genetic engineering than I would about organ printing. Genetic engineering is going to potentially change the entire person’s genetic code and that of their descendants as well,” he said.
He added that fears of medical innovations leading to unnatural physical enhancements of a new class of humans with superior health and abilities were nothing new.
“The choices made by biotechnologists setting out to create a 3D-printed heart could possibly lead to research and technology that could serve a eugenic function. but that’s always been the case. Think about when glasses were invented. What if people said, ‘oh my gosh now we’re going to have a class of people who can see better.”
“It’s not the medical technology itself that has that moral risk,” he said. “It’s the people who have that moral risk.”
As reported by The Times of Israel
